What is Medicare Part C?
KEY POINTS
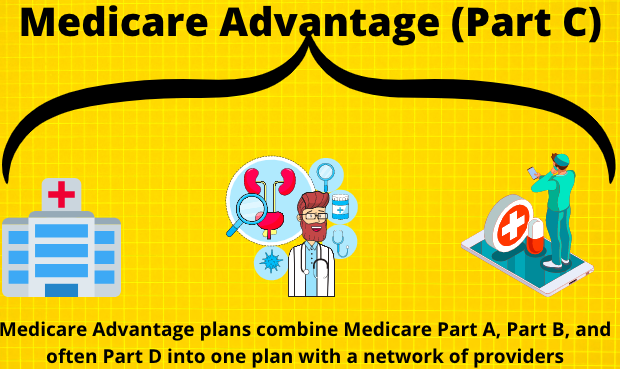
Medicare Part C plans, also known as Medicare Advantage, are an alternative way to receive your Medicare benefits, and they can bundle drug coverage.
Most Advantage plans have low premiums and maximum out-of-pocket limits.
You can only apply for a Medicare Part C plan during an available election period.
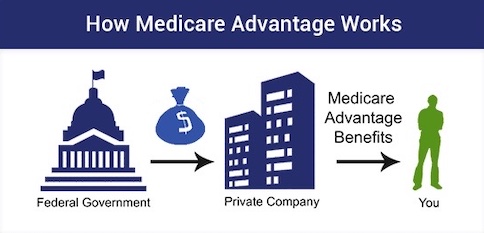
If you enroll in a Medicare Advantage plan, you receive your Medicare benefits through a private insurance company instead of the Federal Government
What is Part C of Medicare? Medicare Part C is not a program that you enroll in at Social Security. Instead, it is the official name for the program we now know as Medicare Advantage (MA).

What is Medicare Part C?
Medicare Part C is not a separate benefit. Part C is the part of Medicare law that allows private health insurance companies to provide Medicare benefits. These Medicare private health plans, such as HMOs and PPOs, contract with the federal government and are known as Medicare Advantage Plans. If you want, you can choose to get your Medicare coverage through a Medicare Advantage Plan instead of through Original Medicare .
If you join a Medicare Advantage Plan (like an HMO, PPO, or PFFS), you will not use the red, white, and blue card when you go to the doctor or hospital. Instead, you will use the membership card your private plan sends you to get health services covered. You will also use this card at the pharmacy if your health plan has Medicare prescription drug coverage (Part D).
Think of Medicare Advantage plans as a package where you will have Part A, Part B, and usually Part D together in one plan. You will have one ID card that you use at the hospital, doctor’s office, and pharmacy. Most types of Medicare Advantage plans include a built-in Part D drug plan, although, in some areas, you can find them without Part D.
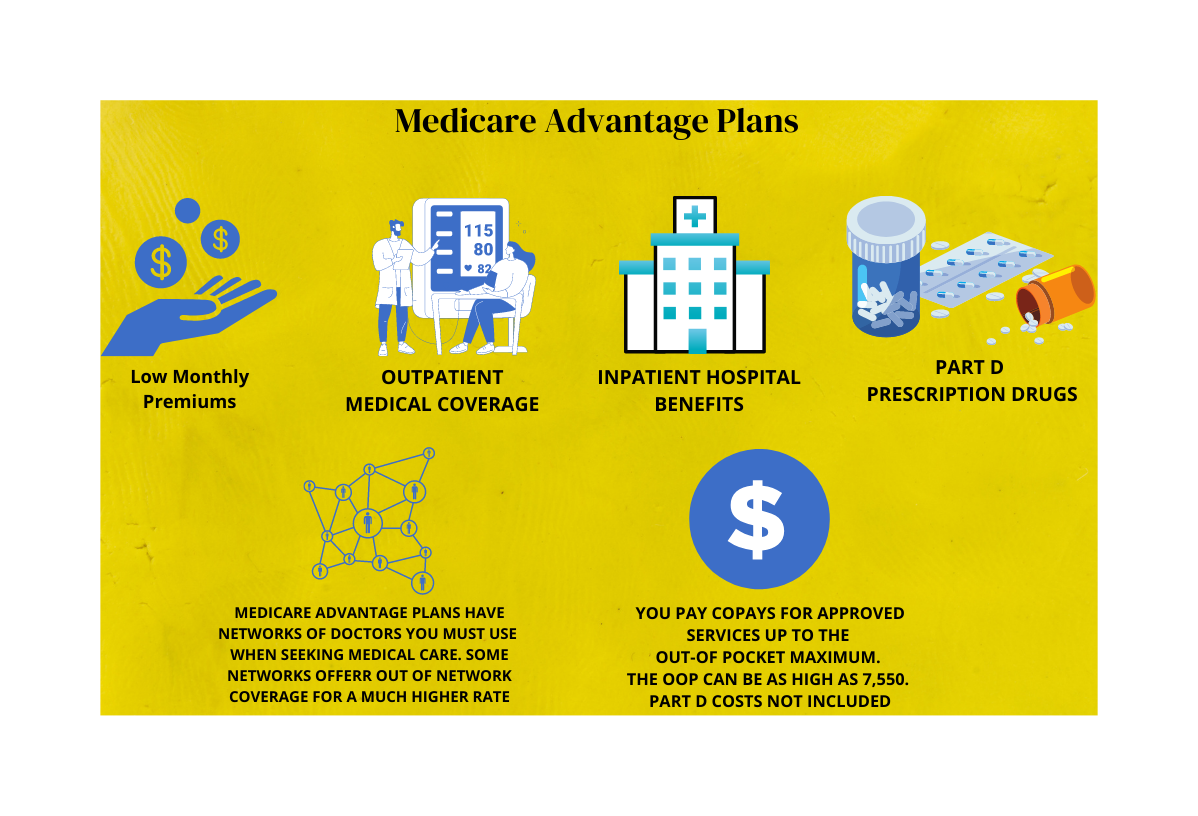
MA plans resemble group insurance benefits you may have had through former employers. Generally, there is a local network of providers that you will use. You will pay copays for many routine services like doctor’s visits, lab work, ambulance, surgeries, hospital stays, urgent care, and more.
What Does Medicare Part C Cost?
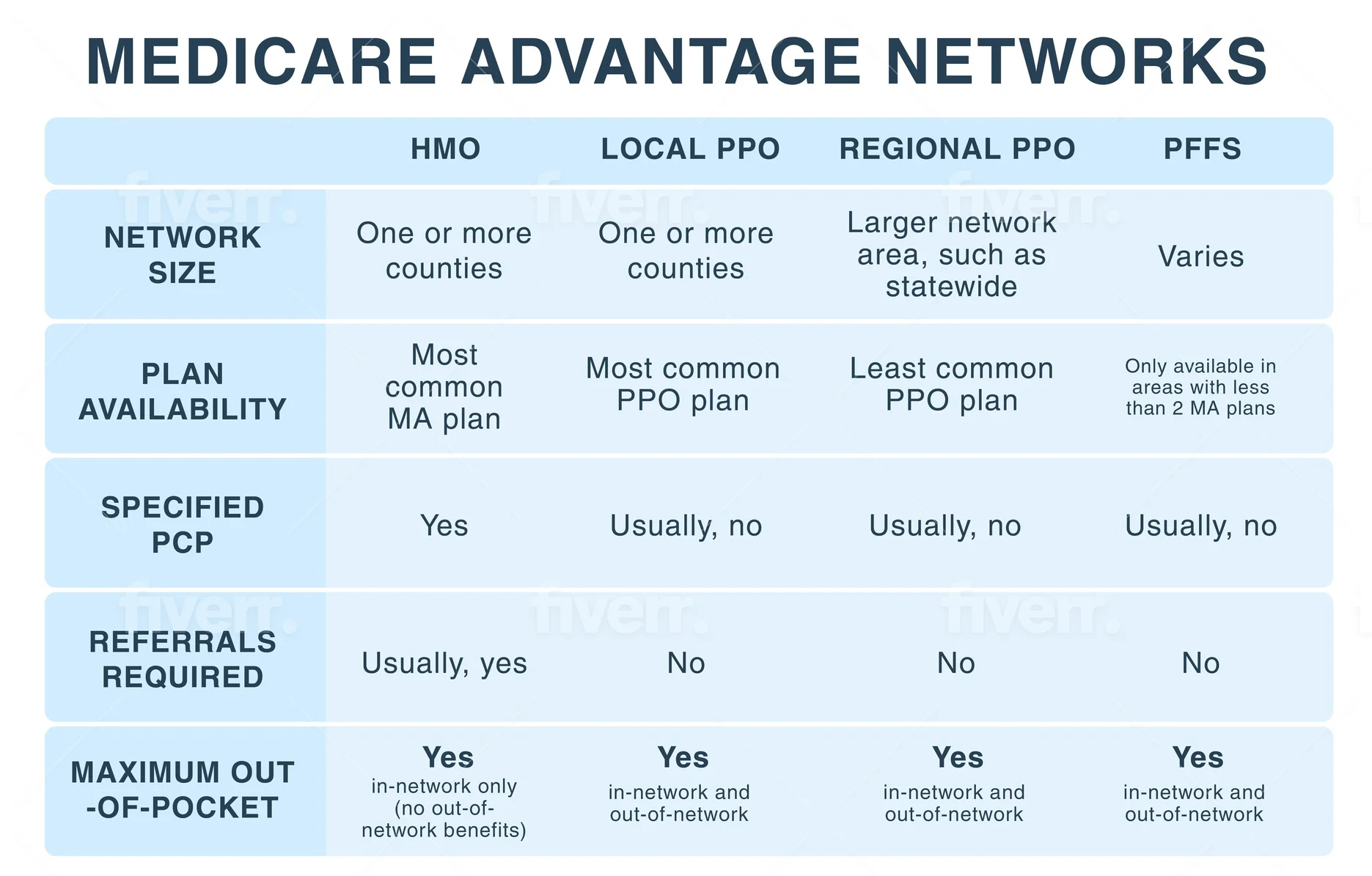
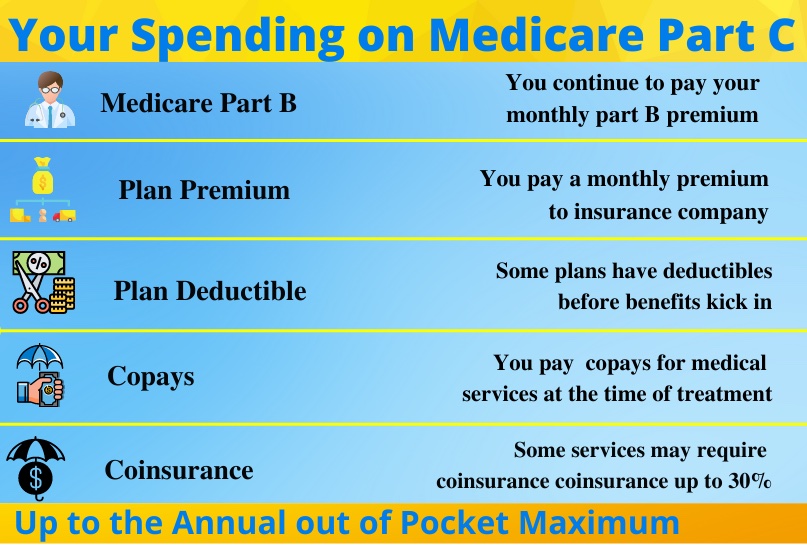
Medicare Part C plans generally have lower premiums than Medigap plans. This is because you are agreeing to treat in the plan’s network and pay copays as you go. The network may be an HMO network, where you’ll need to choose a primary care physician and get referrals.
There are also Medicare PPO and Medicare PFFS options, which have some out-of-network benefits. Besides your monthly premium, your spending might include deductibles, copays, and coinsurance up to the plan’s out-of-pocket maximum.
6-Day New to Medicare Mini Video Course
Lorem ipsum dolor sit amet, at mei dolore tritani repudiandae. In his nemore temporibus consequuntur, vim ad prima vivendum consetetur. Viderer feugiat at pro, mea aperiam
Some Medicare Part C plans have premiums as low as $0. This does not mean that Medicare Part C is free. When you enroll in a Medicare Part C Advantage plan, Medicare pays a fixed monthly sum to the insurance carrier to provide your care. The MA company will offer you a monthly premium as low as possible to attract you to their plan.
The premiums, copays, benefits, and drug formulary can and do change from year to year. This is because the Medicare Part C plan must renew its contract with Medicare annually.
Medicare Advantage Out-of-Pocket Maximums
Every Medicare Part C plan must have an out-of-pocket maximum to protect you. Medicare sets the highest allowable amount for this OOP maximum each year. The Medicare Advantage OOP in 2024 is $8,850. This means that the most you will spend on that plan for Part A and B services is $8,850 (Part D spending is separate.) You will find many Part C Medicare plans that match this, but plans can also set a lower OOP maximum.
When reviewing a potential Medicare Part C plan, look at the OOP maximum on that plan. If you have a year of bad health with lots of spending on copays and coinsurance, do you have enough set aside in a rainy-day savings fund to meet that maximum? If not, find a plan with a lower out-of-pocket maximum, or choose Medigap, which has far less spending on the back end.
Many people ask us to compare Original Medicare vs Medicare Advantage plans. Original Medicare does not have any OOP maximum to protect you. You could pay that 20% forever. So if you cannot afford the more comprehensive Medigap plans, then a Medicare Part C plan at least has an OOP cap to protect you. For many folks, this makes what Medicare Part C covers a more attractive option than Original Medicare alone.
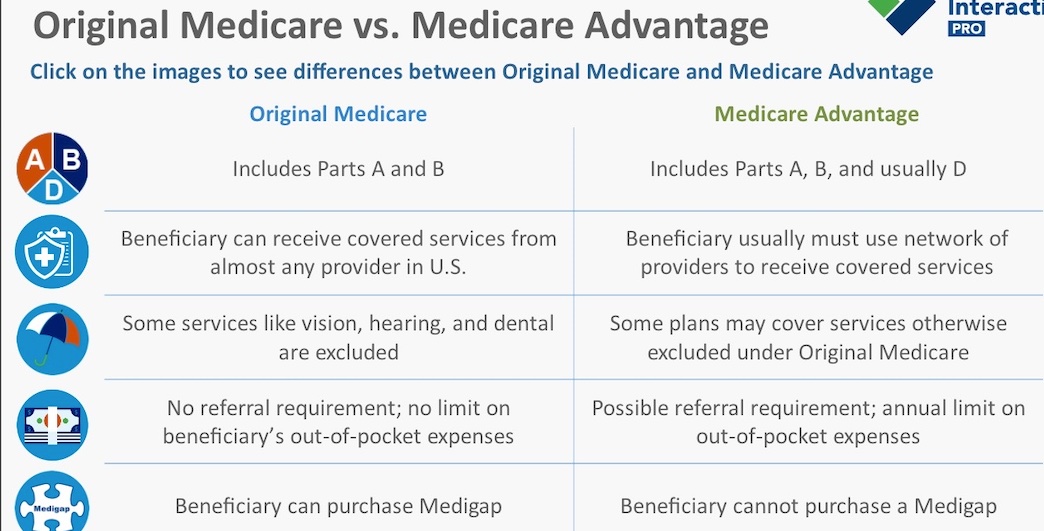
Medicare Advantage Plans must offer, at minimum, the same benefits as Original Medicare (those covered under Parts A and B) but can do so with different rules, costs, and coverage restrictions. You also typically get Part D as part of your Medicare Advantage benefits package (MAPD). Many different kinds of Medicare Advantage Plans are available. You may pay a monthly premium for this coverage, in addition to your Part B premium.
6-Day New to Medicare Mini Video Course
Medicare Part C Eligibility
Who is eligible for Medicare Part C? Any Medicare beneficiary, regardless of age, can purchase a plan if they meet these criteria:
- You must be enrolled in both Medicare Part A and B. Many people mistakenly think they can drop Part B if they enroll in a Medicare Part C plan. This is NOT the case. If you drop Part B, you will immediately be kicked out of your Part C plan.
- You need to live in the plan’s service area. This Medicare Part C eligibility will be based on the address that you have on file with Social Security. You must choose a plan that operates in that same county. Some plans will be specific to only one or two counties, while others might span the whole state.
Be sure to also remember that Medicare Advantage plans have election periods. This means that you can enroll during your Initial Enrollment Period or during the Annual Election Period in the fall. There are also certain Special Election Periods (SEPs) in certain circumstances, such as if you move out of state and lose your plan. You would then be granted a SEP to enroll in a plan mid-year in your new state.
What Does Medicare Part C Cover?
Medicare Part C covers what Part A and B do when you have Original Medicare. You will have both hospital and outpatient benefits. However, instead of paying deductibles and 20% of your medical services, you will pay the plan’s copays.
Each Medicare Advantage plan has a summary of benefits. This summary lists various medical services. The summary will show you what your copay or coinsurance will be for each service. For example, you might pay $10 for lab work, $50 for a specialist visit, $300 for an MRI – and $400 copay for hospital stay for days 1-4 and so on…
Some items might have a $0 copay. That means you will have no copay for that service. The highest amount that you will pay in the network for any service is 20%. We typically see a 20% coinsurance requirement for things like durable medical equipment, dialysis, chemotherapy, and radiation in many plans. Review your summary of benefits carefully to see what you can expect to pay for these and other items.
Remember that everything you spend on Part A and B services counts toward your out-of-pocket maximum. If you hit that maximum, your Part C plan will pay 100% after that for the rest of the year.
MA plans often include a built-in Part D drug plan.
Do I need Medicare Part C?
Part C is optional, voluntary coverage. You get to choose whether you want to enroll in Original Medicare or would prefer a Medicare Advantage (Part C) plan instead. It is up to you to decide what is the best fit for you. However, MA plans provide you with a cap on your expenses, whereas Original Medicare does not limit your costs.

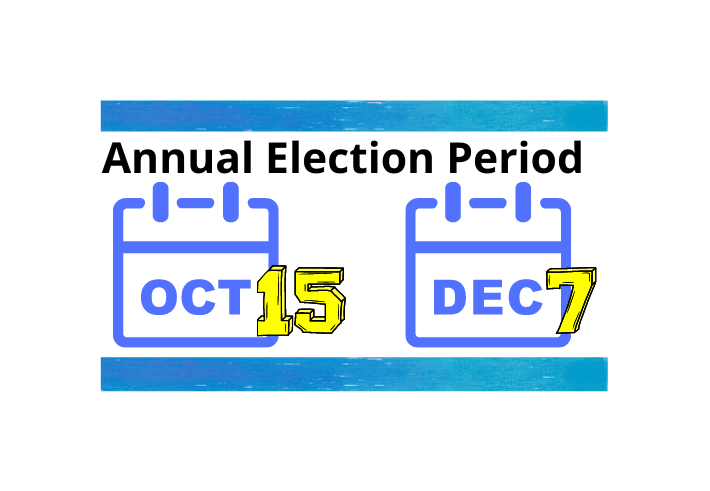
Medicare Part C Enrollment Periods
Unlike Medigap policies, you can only enroll into or dis-enroll from a Part C Medicare plan during certain periods. You can enroll in a plan during your Initial Enrollment Period when you first get Part B. You can also change during the Annual Election Period each fall, which runs from October 15 – December 7th, with your benefits beginning January 1st.
The Annual Election Period exists because if you are enrolled in Medicare Part C or Part D, your plan’s benefits, formulary, pharmacy network, provider network, premium and/or co-payments, and co-insurance may change on January 1 of each year. Medicare wants you to have an opportunity to change your plan if you don’t like the changes coming for next year.
There are also special election periods for Medicare Advantage plans, such as when you leave employer group coverage or move out of your plan service area. You can learn more about these here. A good insurance agent who specializes in Medicare-related insurance products can help you as a beneficiary learn who qualifies for Medicare Advantage and the enrollment periods available.
Part C Medicare Help
Medicare Advantage plans have specific rules, networks, and enrollment periods. Limitations, restrictions, and copays may apply. Working with a licensed insurance agent can help you understand what is a Medicare Advantage plan and the additional information you may need before you apply for a plan.
Do you need assistance regarding how to get Medicare Part C and in choosing a plan that will be accepted by your doctor and provide affordable benefits to you? We are happy to help – call (843) 227-6725
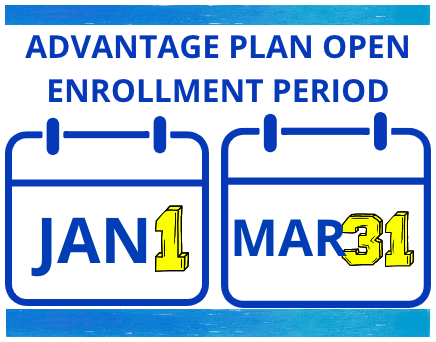
Fall Enrollment Period is the time to change advantage or drug plans
Advantage Plan Open enrollment period allows ONE last change in advantage plans
Key Takeaways
- * When you enroll in a Medicare Advantage plan, you choose to receive your Medicare benefits through your plan.
-
- * You continue to pay the Part B premium, but you generally have a lower monthly premium and a maximum out-of-pocket
- limit on your costs.
-
- * As long as you are enrolled in Part A and Part B, you can apply for a Medicare Advantage plan during an available election period window.

