Key Points
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
Private, for-profit plans often require Prior Authorization. Medicare Advantage (MA) plans also often require prior authorization to see specialists, get out-of-network care, get non-emergency hospital care, and more. Each MA plan has different requirements, so MA enrollees should contact their plan to ask when/if prior authorization is needed.
Traditional Medicare, historically, has rarely required prior authorization. Originally, the Social Security Act did not authorize any form of “prior authorization” for Medicare services, but the law has subsequently been changed to allow prior authorization for limited items of Durable Medical Equipment and physicians’ services. Despite this change, there are still very few services requiring Prior Authorization in traditional Medicare.*
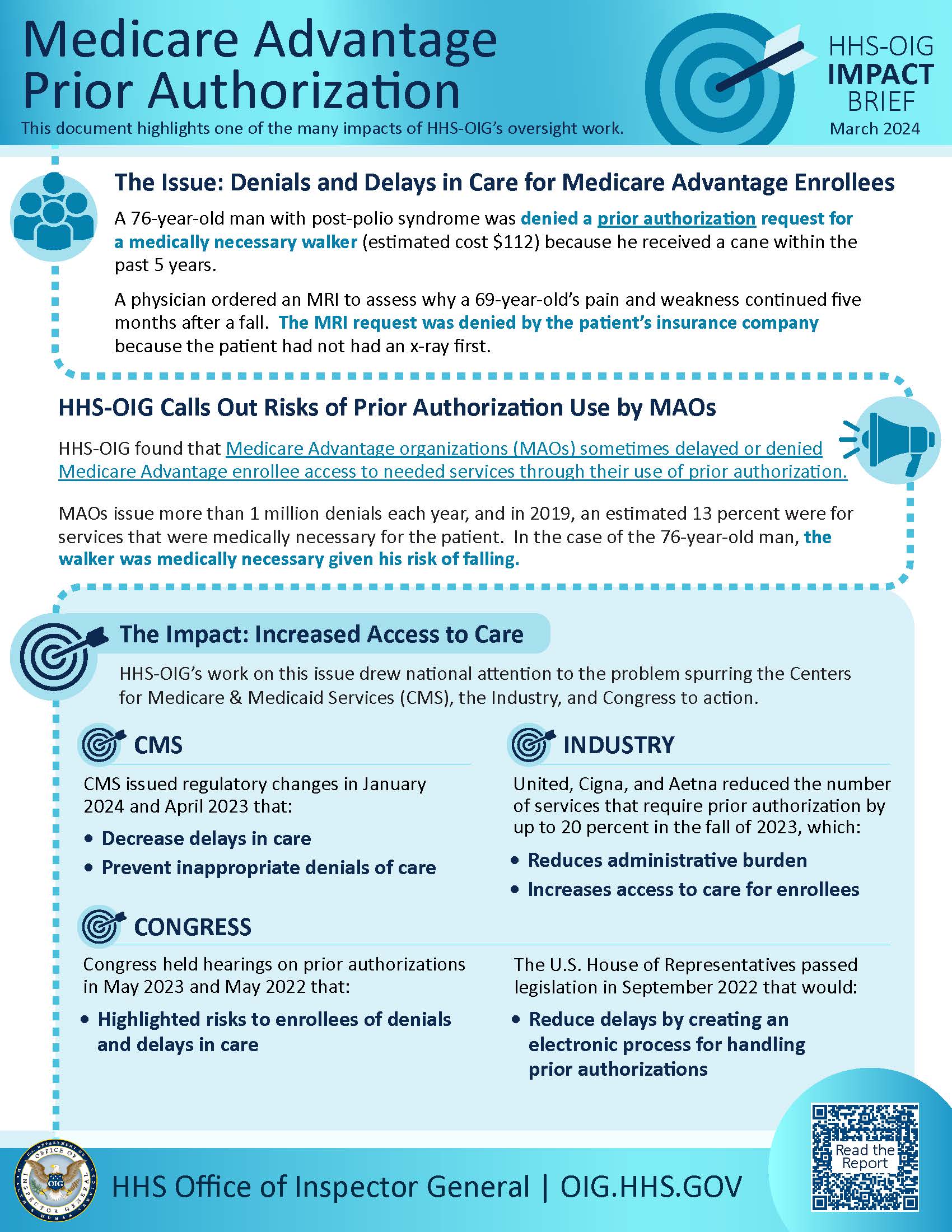
Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care.
Although Medicare Advantage is supposed to offer the same benefits as Original Medicare, that’s not exactly the case. Why?
- 1) WITH ORIGINAL MEDICARE -YOUR RED WHITE AND BLUE MEDICARE CARD YOU GOT WHEN TURNING 65- YOU CAN GO TO ANY DOCTOR IN THE US THAT ACCEPTS MEDICARE 98% ACCEPT IT. THE MAYO CLINIC ACCEPTS ORIGINAL MEDICARE AND ALL SUPPLEMENTS THAT PAY WHAT MEDICARE DOES NOT PAY.
WITH MEDICARE ADVANTAGE PLANS HAVE RESTRICTIVE HMO STYLE NETWORKS. YOU LOSE THE ABILITY TO SEE THE DOCTORS YOU WANT TO WHEN JOINING ADVANTAGE PLANS. PRESTIGIOUS MEDICAL GROUPS LIKE THE MAYO CLINIC DO NOT, LET ME REPEAT, DO NOT ACCEPT MEDICARE ADVANTAGE PLANS - ***INTERESTING FACT” Nearly half of Medicare Advantage plan directories contained inaccurate information on what providers were available, according to the most recent federal review. .
- ETRITIJGIP
- 2) WITH ORIGINAL MEDICARE, WHEN YOU DOCTOR PRESCRIBES AN MRI, SURGERY, OR SKILLED CARE THEN MEDICARE PAYS FIRST AND THE SUPPLEMENT PAYS THE REST.
WITH MEDICARE ADVANTAGE PLANS, WHEN YOUR DOCTOR RECOMMENDS ANY PROCEDURE THAT MAY COST THE INSURANCE COMPANY A GOOD AMOUNT OF MONEY, THE INSURANCE COMPANY “EXPERTS” CAN OVERIDE YOUR DOCTORS DECISION AND DENY THE PROCEDURE YOU OWN DOCTOR RECOMMENDS. THE PRIVATE INSURANCE CAN DENY A CLAIM YOUR DOCTOR PRESCRIBED. -
- ***INTERESTING FACT: High overturn rates of appealed denials, and widespread and persistent CMS audit findings about inappropriate denials, raise concerns that some Medicare Advantage beneficiaries and providers were denied services and payments that should have been provided. This is especially concerning because beneficiaries and providers rarely used the appeals process designed to ensure access to care and payment, appealing only 1 percent of denials during 201416. Although CMS takes a variety of compliance and enforcement actions against MAOs when it identifies problems, more action is needed to address these critical issues.
-
- 3)
3
-
H
WIT
The Doctors Opinion on Medicare Advantage Plans
Medicare Advantage Plans Being Sued for Fraud
Shortcode is empty